Relapses and infections
Infections, both viral and bacterial infections, are a known trigger of relapse. You are more than twice as likely to have a relapse in the week prior to, or the 5 weeks after, an infection. We are also continuously being exposed to new viruses that infect us but don’t necessarily cause symptoms. An example of this is the JC virus that causes PML (progressive multifocal leukoencephalopathy) a rare complication of immunosuppressive therapy. When we initially become infected with the JC virus it does not cause any symptoms; it simply gets into our body and persists. It persists as an asymptomatic lytic infection. In the majority of us, persistent JC virus infection doesn’t cause any problems. Only if we become immunocompromised do we have a chance of this virus mutating and causing PML.
Similarly, for the majority of us when we get infected with Epstein-Barr virus (EBV) it does not cause symptoms; only the minority of us get glandular fever or infectious mononucleosis. The same applies to another herpes virus called CMV or cytomegalovirus; asymptomatic infection is the rule. What is interesting about the herpes viruses is that they become latent in the body and reactivate every now and then. These reactivations of latent viruses are usually asymptomatic but are strong enough to stimulate the immune system and may also trigger relapses. There is some evidence that this may actually be the case, which is why there is a compelling case to test antiviral therapies as a potential add-on treatment for MS.
When I did my PhD I studied a marker of immune activation on a daily basis in pwMS over many months. This marker is excreted in the urine in high levels and study subjects diligently collected daily urine specimens for me and kept them frozen in the freezer and brought them to me analyse after a three month period. I found that immune activation usually preceded the occurrence of new MRI lesions by a few weeks. Please remember new MRI lesions are the equivalent of subclinical relapses. I, therefore, proposed in my thesis that latent viral reactivations may be the factor responsible for this immune activation, which then triggers MS disease activity. This is one of the reasons why I am so interested in the viral MS hypothesis.
Virus-induced MS exacerbations don’t have to apply to exogenous viruses only, i.e. viruses that come from outside the body but could also apply to endogenous viruses, i.e. viruses that reside in our bodies or genome. The latter refers to human endogenous retroviruses (HERVs). This is one of the hypotheses that underpin our Charcot Project. Can we treat MS by reducing endogenous viral reactivation (HERVs)? Can we treat MS by preventing the reactivation of latent herpes viruses, in particular, EBV? This is why we are exploring add-on antiviral studies to see if we can prevent MS disease reactivation.
It is very difficult to avoid viral infections. The one thing you can do is have your annual flu vaccine and try to avoid coming into contact with people who are clearly ill and potentially shedding the virus.
Please, note that the observation of infections triggering relapses is not limited to viral infections, but also applies to bacterial infections, in particular, urinary tract infections. This is why it is important to improve the management of bladder problems in people with MS (pwMS) with the aim of preventing or reducing urinary tract infections (UTIs). PwMS with recurrent UTIs do worse than pwMS without UTIs. However, to prevent or reduce the frequency of UTIs you have to know how MS causes bladder problems and to deal with them.
Bladder dysfunction
Bladder dysfunction is the most common symptomatic problem I have to deal with in an MS clinic. More than 50% of pwMS have bladder problems. Bladder dysfunction in pwMS is one of the integrators of early damage, particularly spinal cord damage, and an early read-out of a poor prognosis. I, therefore, take symptoms of bladder problems seriously as it has implications around MS prognosis and its treatment. For example, if you have early bladder symptoms you may want to choose a more effective therapy early on rather than take a chance on a less effective DMT and waiting to see if you are a responder or not.
Why do pwMS who develop bladder dysfunction do worse than those who don’t have bladder symptoms? The bladder is a complicated organ with several neurological components that can be affected by MS and hence is sensitive to damage. The descending nerve fibres that travel from the brain to the lower spinal segments are very long and hence have a greater chance of being affected by MS lesions in their path down to the spinal cord bladder centre in the sacral or lower segments of the spinal cord. The same is true for motor fibres that control movement in the lower legs. The bladder, unlike the motor fibres to the leg, is more complicated because of the need to coordinate the different muscles. Therefore any progressive MS damage is more likely to manifest with bladder dysfunction early on. This is why I now include bladder problems in my list of poor prognostic factors in MS.
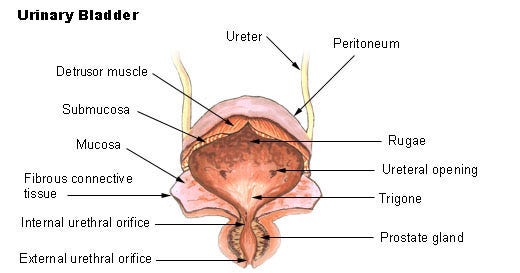
The bladder has two muscles that need to be coordinated in their action for the bladder to function normally. The detrusor or balloon muscle and the sphincter or valve muscles When the bladder is filling up the detrusor muscle has to relax to allow the bladder to expand with urine and the sphincter has to contract to keep the urine in the bladder. The opposite occurs when you pass urine; the sphincter or valve opens and the detrusor contracts to empty the bladder.
Hesitancy
Urinary hesitancy is the symptom you get when the function of the two muscles are not coordinated with each other; i.e. you try to pass urine and the bladder sphincter won’t open. Hesitancy may be intermittent and if you wait or come back later the bladder will open and allow you to pass urine. However, pwMS find urinary hesitancy and its unpredictability very frustrating. The sphincter can also close as you pass urine, which breaks up the urine stream or prevents you from emptying your bladder completely. The latter also causes dribbling. The medical term for incoordination of the bladder muscles is dyssynergia or more correctly detrusor-sphincter-dyssynergia (DSD). The drug treatment for DSD includes the so-called alpha-blockers ( prazosin, indoramin, tamsulosin, alfuzosin, doxazosin and terazosin). Other strategies include small bladder stimulators or vibrators; these are placed over the pubic area and work by blocking signals that inhibit the sphincters. The vibrators work in some pwMS and may help relax the sphincter. It is also important to try and relax when passing urine; this often helps improve hesitancy. The sound of running water, for example from a tap, may trigger the relaxation of the sphincter. This can be a problem in public toilets when opening a nearby tap may not be possible or appropriate. Some pwMS find pressing on the lower abdomen helps. If all else fails regarding urinary hesitancy, intermittent self-catheterisation (ISC) may be the only option.
Frequency
In MS the commonest bladder problem is spasticity, or irritability, of the detrusor muscle. The detrusor can’t relax and this prevents the bladder from filling to its maximum capacity. Frequent spasms of the detrusor muscle tell the brain that it is full and you need to go to the toilet. This causes frequency; i.e. the need to go to the toilet many times during the day and night. Frequency often goes with the symptom of urgency, the need to get to the toilet as quickly as possible to prevent yourself from being incontinent.
Incontinence occurs as you often lose the ability to suppress or ignore the signals from the detrusor muscle and the sphincter relaxes or opens as part of a spinal cord reflex. We typically treat this problem with the so-called anticholinergic drugs, for example, oxybutynin, solifenacin or tolterodine. The older generation anticholinergics such as oxybutynin cross the blood-brain barrier and enter the brain where they can exacerbate cognitive problems in pwMS. This is why I avoid using them. The commonest side-effect of anticholinergics is dryness of the mouth and they can make constipation worse. There is also a risk that they will relax the bladder too much and precipitate urinary retention. All pwMS must be warned about this problem when starting anticholinergics; I have several pwMS under my care that go into retention when they use anticholinergic drugs. The solution to the latter is again ISC.
The good news is that we now have a relatively new muscle relaxant mirabegron (Betmiga), which works by activating the β3 adrenergic receptor in the detrusor muscle. I am increasingly using mirabegron to avoid the side effects associated with anticholinergics.
Urgency
When urgency is a problem, trying some distraction techniques such as breathing exercises and mental tricks (for example, counting) to take your mind off the bladder may be helpful. If urinary frequency is your main problem you may want to try and retrain your bladder by holding on for as long as you can each time before passing urine. The aim is to train the detrusor muscle to expand more so that it can hold on for longer when you need to go to the toilet. In my experience these behavioural techniques rarely work for long; MS is a relapsing and/or progressive disease and in all likelihood, the bladder pathways will be affected more due to the development of new lesions or the expansion of old lesions.
If you fail to respond to anticholinergics and/or mirabegron and behavioural techniques you need to have your bladder scanned to see if you have a raised residual volume. The residual volume is the amount of urine left behind after you have emptied your bladder. If the residual volume is greater than 80-100mL you may need to consider intermittent self-catheterisation or ISC. ISC serves two purposes; it increases your so-called functional residual bladder volume allowing more storage space for urine in the bladder; this reduces frequency and urgency. This can help you if you have to take a long trip or to get through a social activity without having to pass urine. It also helps reduce nocturia or having to get up frequently at night to pass urine. You will be surprised how much better you feel if you get a good night's sleep. Reducing nocturia and improving sleep may also improve MS-related daytime fatigue.
Another treatment that is becoming increasingly common is botox of the detrusor muscle. This paralyses the muscle turning it into a flaccid bag for urine storage. Almost all pwMS who have detrusor botox injections are using ISC. In the past, before botox was available, there were surgical techniques that could be used to denervate or remove the nerve supply to the bladder that had the same effect; these techniques are now rarely used.
ISC also removes urine from the bladder. This is important if you are having recurrent bladder infections. The residual urine acts as a culture medium for bacteria and by clearing your bladder you can prevent bladder infections. The opposite can occur. If you don't get the ISC technique correct you can introduce bacteria into the bladder that then cause infections.
Percutaneous tibial nerve stimulation (PTNS) or posterior tibial nerve stimulation, is a form of neuromodulation that can help with neurogenic bladder and may improve urinary urgency, urinary frequency and urge incontinence. It is offered as a treatment in specialist neuro-urology units.
UTIs and disease progression
The more infections you have, in particular, severe infections, the more likely it is your MS will progress. Therefore if you have recurrent bladder infections you should try and prevent them from occurring. How do you do this? Drink lots of liquids; flushing the bladder reduces infection rates. Also changing the pH of your urine by drinking citric acid (citro soda or lemonade) also helps. It is likely that both alkalinization and acidification of your urine may work depending on the bacterial species colonising your bladder. Cranberry extract, which contains proanthocyanidins, a substance that reduces bacteria from colonising the bladder may help. Please note you need to use the extract and not the juice as the proanthocyanidin concentration in the juice is too low to have an effect.
An infrequently used option is a bladder instillation with a liquid containing sodium hyaluronate (Cystistat), which replaces the glycosaminoglycan (GAG) layer or glycocalyx of the bladder wall. This layer makes it difficult for bacteria to stick to the wall to cause infections and is one way of preventing bacterial biofilms, or slime, from forming. Biofilms are increasingly being recognised as a major problem as they prevent antibiotics from reaching the bacteria to kill them and act as a nidus for recurrent infections. I have a few patients who have used Cystistat with dramatic results.
Increasing the frequency of ISC may also help reduce recurrent UTIs. Finally, using urinary antiseptics may help reduce infection rates. Urinary antiseptics are antibiotics that are concentrated in the urine; they are given in low concentrations so they have little impact on the rest of the body. I tend to cycle their use, every 3-4 months, to prevent the bacteria in the bladder from becoming resistant to a specific antibacterial. The agents I use currently are trimethoprim, cephalexin and nitrofurantoin. Methenamine is another urinary antiseptic but is not readily available in the UK due to supply issues. Another one that may still be used in some countries is nalidixic acid, but it has been taken off the market in the UK because of adverse events, i.e. weakening and rupture of muscle tendons. The latter is a class effect of the oxolinones and related antibiotics.
Nocturia
If nocturia is your main problem, using agents to concentrate the urine at night might help. There is a hormone called DDAVP that works on the kidney to reduce urine production. You can take DDAVP as a nasal spray or tablets. DDAVP can only be taken once a day; if you use it continuously your kidneys will retain water continuously and this can be very dangerous. The latter is called water intoxication; it presents as swelling of the feet and reduces the salt or sodium levels in your blood. If blood sodium level becomes too low it can cause problems. This is why when you start using DDAVP you need to have your sodium levels checked about 4-6 weeks after starting therapy.
I am not sure why, but some neurologists are reluctant to prescribe DDAVP. This is a shame as it is a very good drug and can make the difference between getting a good night's sleep or waking feeling tired. You can use DDAVP intermittently and you can use it during the day, for example when you need to go on a long trip or for social occasions, e.g. going to the movies or theatre. You can only use DDAVP once a day. The most common side effect is swelling of the feet; it happens in approximately a third of pwMS and is more common in pwMS who are less mobile.
Other advice I give to pwMS is that if you are a smoker then stopping smoking may significantly improve your bladder symptoms; nicotine irritates the bladder. Similarly, reducing alcohol and caffeine consumption may also help; both these agents affect the kidneys and cause them to make more urine. Medically this is referred to as diuresis; both nicotine and caffeine are diuretics.
Try to anticipate times when urinary frequency and urgency are likely to be most inconvenient; reducing the amount that you drink beforehand may help. For example, when you go out, don’t drink much for 2-3 hours before you go out. However, do not reduce your total fluid intake to less than 1.5 litres each day. After you have finished passing urine, go back to the toilet again after a few minutes to try to pass some more urine. This is called the double micturition technique, which aims to make sure the bladder is emptied completely.
Finally, if all else fails some pwMS may need to be permanently catheterised. This can be done via the urethra or the lower abdominal wall. The latter is called a suprapubic catheter. Being permanently catheterised sounds awful, but in some pwMS, this drastically improves their quality of life. I have several pwMS who have let bladder dysfunction control their lives and as a result, they have become socially isolated. They are typically anxious about being incontinent in public. To avoid this possibility they choose to stay at home. This is clearly unnecessary and with the strategies highlighted above adequate bladder control should be the norm in MS.
In my experience, the biggest hurdle to achieving adequate bladder control is pwMS accepting their bladder symptoms as being part of the disease and living with them. These patients often take to using continence pads and adult nappies/diapers as is if this was normal for someone with MS. This is not normal; living with incontinence is not ideal. People who are incontinent and disabled are more likely to get skin rashes and pressure sores. These complications are related to being wet or damp most of the day. Please don’t accept this as being normal or something you have to live with. If you have problems, tell your MS nurse or neurologist; they will be able to help you.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.





Wow, I have never read a thorough detailed well-written article on bladder problems such as this one! I recognized myself in many of the above problems, but taking Betmiga mostly solved the problem of frequency, and pressing on my lower abdomen is daily routine for hesitancy. However, UTI after sex remain. I've had UTIs after sex for the past 12 years (since I first started having sex), and I've had only one partner so far - my husband. I've managed to keep them under control eventually, by taking cranberry products with PAC and taking d-mannose, however, this summer I developed some form of urinary retention - when I pee I have to press on my lower stomach, and only then I have the feeling that the bladder is empty. It obviously isn't, because UTI follows within 24h of sex. The only thing that works now is taking a single antibiotic after sex. :( That is not a long-term solution. Have you had any female patients with similar problems, and did they have any luck in resolving their problems? Take care!
Excellent article on bladder problems - thanks.
I've been taking Hiprex for about 18 months and it's changed my QOL as i used to get UTIs every 2 or 3 months and was. building up resistance to antibiotics. You talk about the risk of building up microbial resistance if taking methenamine hippurate. continuously and advise having 'fallow periods'. On past performance I'd very likely get a UTI which would be very unwelcome which would probably see me in A&E. I know people who've been taking Hiprex for 10-15 years with no. resistance problems. How strong is the evidence and thoughts?