Has MS affected your cognition?
MS is not only a physically disabling disease it also affects cognition. However, there is something you can do about it, which is why you need to use it or lose it.
I often use the term advanced MS to describe people with MS who have had the disease for some time and are disabled. The reason for doing this is that the term is relatively neutral, captures people with both relapse-onset and primary progressive MS and doesn’t necessarily affect access to disease-modifying therapies (DMTs). As soon as you label someone as having secondary progressive MS it closes down the treatment options for their MS. For example, in the NHS siponimod is the only DMT that is available to treat people with SPMS and even then it is limited to people with active SPMS, which represents a very small proportion of the population of people with SPMS.
To find out if you have advanced MS you probably need to put yourself through a battery of so-called stress tests to find out much reserve you have left to deal with MS and the ageing process in the future. I try not to define advanced MS using the EDSS as it entrenches the physically disabling, particularly lower-limb function, worldview of MS. Advanced MS is really when someone has lost reserve in a particular neuronal system and they are noticing worsening in that system that is impacting on their ability to function at a personal, social or occupational level and by inference is affecting their quality of life.
Using this definition someone can have advanced MS with very little physical disability. As you are aware the impact of MS may be cognitive, which is the main driver of the high early unemployment rates we see in MS. In Europe close to 50% of pwMS are unemployed 10 years after diagnosis with an average EDSS of 3.0-3.5; an EDSS level that is not associated with outward signs of physical disability.
A software engineer with MS who depends on her cognitive skills for writing computer code needs to be able to concentrate for prolonged periods of time with multitasking. Even with subtle cognitive impairment, she may find it very difficult-staying at the top of her game. She will notice much earlier her progressive cognitive loss based on her performance or lack of performance at work. In comparison, a professional athlete may not necessarily notice early cognitive impairment but will be more susceptible to the effects of MS on their coordination and endurance, for example, the marathon runner with a dropped foot.

These examples are the two extremes, but they illustrate why we need stress tests of the nervous system to be able to ascertain how much reserve there is which will give us some idea of how advanced MS is in a particular domain. One thing that is not done very well in MS clinics is cognition. Most MS centres don’t have the resources to monitor cognition properly. This clearly needs to change.
In almost every MS clinic I do I see patients who complain of cognitive symptoms; increasing forgetfulness, difficulty multitasking, the inability to learn and use a new technology or cognitive fatigue. Some of you may relate to these symptoms.
One of my high functioning patients, who worked in a large City law firm, simply could not keep up and was forced to take early retirement because of her MS. She had been interferon-beta-1b for 12 years but had stopped treatment about 7 years ago when she had moved to London. Her MRI showed a highish lesion load and severe brain atrophy or volume loss. She had had a few relapses on interferon-beta in the early years, but her neurologist decided to leave her on interferon-beta. Back then this was normal practice; we didn’t expect interferon-beta to render you relapse-free. Interferons were only meant to reduce attack rates by about a third and severe attacks, i.e. those requiring steroids and/or hospital admission, by about a half. The only alternative when this patient was having relapses on interferon-beta was glatiramer acetate; this was in the pre-natalizumab era.
Apart from her cognitive problems, this patient had mild unsteadiness of gait, but this had not affected her walking distance and she was still able to do yoga several times per week. To help with her unemployment insurance claim I requested a formal neuropsychological assessment and she was documented to have profound cognitive deficits across multiple domains. The conclusion based on these tests was that she would never be able to have meaningful employment again; at least not in the knowledge economy. When I took a detailed history it was clear that she had had progressive cognitive impairment over at least 7-10 years. In other words, she had advanced (secondary progressive) MS manifesting as progressive dementia.
This patient is not unusual. You therefore must not underestimate the impact MS has on cognition. Cognitive problems can be there from the start; approximately a quarter of people with a radiologically isolated syndrome (RIS) or asymptomatic MS already have cognitive impairment. The proportion of people with cognitive impairment gets higher the longer you have the disease. What is driving cognitive impairment is almost certainly grey matter pathology, both in the cortex and deep grey matter of the brain, which is not really visible with our current MRI monitoring tools.
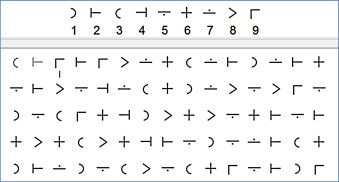
Until recently the MS community used the Paced Auditory Serial Addition Test (PASAT) for monitoring cognition in clinical trials. The PASAT is a measure of cognitive function that assesses auditory information processing speed and flexibility, as well as calculation ability. The PASAT is presented using audiotape or disk to ensure standardization in the rate of stimulus presentation. Single digits are presented every 3 seconds and you have to add each new digit to the one immediately prior to it. Shorter inter-stimulus intervals, e.g., 2 seconds or less have also been used with the PASAT but tend to increase the difficulty of the task. The PASAT is a very difficult test because it requires multitasking and activation of many areas of the brain. In short, the PASAT is a very good cognitive stress test.
One of the reasons the MS community has dropped the PASAT test in trials is because of the learning effect. When you do the PASAT test your scores improve because of so-called ‘learning’ or ‘practice’ effects. In reality, this is a general phenomenon for most neurological stress tests; our nervous systems are wired for learning and wired for improvement. In several clinical trials, we have shown that not being able to improve on the PASAT at the beginning of the trial predicted a worse outcome during the trial. In other words, pwMS who can’t learn i.e. were unable to improve their PASAT scores, do worse and these observations are independent of treatment. However, those on a DMT do better than those not on a DMT or a placebo.
Not surprisingly, pwMS who were poor learners are older, have a higher disability score at baseline, smaller brains and higher lesions volumes on MRI; i.e. they have reduced cognitive reserve or resilience. In other words, these people have more advanced MS.
People with advanced MS with the reduced reserve are primed to continue to deteriorate despite being on a DMT. The previous damage or smouldering MS is driving this worsening. This may explain why the treatment response to DMTs drops off with ageing and disease duration. Please note this applies to all DMTs, including the top guns such as alemtuzumab and HSCT.
It is important to try and prevent this by treating MS as early and effectively as possible. Some pwMS are luckier than others; i.e. you may present very early in the course of your MS before too much end-organ damage has accrued. In others, the asymptomatic period of the disease may be longer, during which time you acquire a lot of end-organ damage. Regardless of what group you are in, you need to make sure you are on top of your MS disease activity. This is why we now treat MS to a target of no evident inflammatory disease activity (NEIDA).
It is clear from several data sources that on average pwMS do best on DMTs that have the greatest impact on inflammatory activity (new MRI lesions and relapses) and those that reduce brain volume loss. In reality, these are the high and very high efficacy DMTs. This is why flipping the pyramid and going for the most effective DMTs first-line is a very appealing treatment strategy; particularly the DMTs that ‘normalise’ the rates of brain volume loss.
This Newsletter illustrated why we should be monitoring cognition in routine MS clinical practice. Although this topic gets discussed and debated frequently, many neurologists don’t agree with doing routine cognitive testing, because of the lack of evidence that DMTs and symptomatic treatments impact cognition. This, however, is changing as there is some data emerging that DMTs have positive effects on cognitive function, even in advanced MS. For example, siponimod has been shown to delay cognitive worsening compared to placebo in people with SPMS.
Prior to COVID-19, we had started doing annual SDMT (symbol digit modalities test) in outpatients on all of our patients attending the clinic. This stopped with our virtual consultations, but it can potentially be done online. The SDMT is a sensitive measure of impaired cognition in people with MS. The SDMT is primarily a cognitive reaction time test or information processing speed but relies on visual scanning and oral ability.
Would you want to know what your SDMT score is? Having a score may motivate you to improve it by doing cognitive rehabilitation. Yes, cognition is no different to physical functioning; if you don’t use it you lose it. This is why education and performing cognitive tasks such as playing bridge, doing sudoku and crossword puzzles, learning a second or third language, etc. have been shown to delay the onset of dementia. These tasks are to cognition what exercise is to physical function. So get exercising, exercising your brain.
I have been involved in a #ThinkCognition campaign in the hope of shifting the MS worldview from a physical one to a cognitive one. By treating cognition with the same level of importance as physical functioning we will hopefully get the MS community to be more proactive when it comes to managing MS.
Please share your thoughts on the issues raised in this newsletter, particularly advice you may have for other readers who have MS.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.
Subscriptions: Funds from the MS-Selfie Newsletter subscriptions, which will provide you access to the Newsletters on case studies will be used to administer the site; i.e. to pay for a part-time administrator to proofread the Newsletters, manage the workflow and curate and transfer the contents of the Newsletter onto the companion MS-Selfie microsite. Funds will also be used to compensate future guest writers and if sufficient to support MS research in the future.




Some years ago when she was on a course about brain function/deficits, my neuro physio was shown examples of MRI activity of people doing active language work - i.e. not practising a language they knew but engaged in new learning. She said it was astonishing - so many areas of the brain lit up. She was told that the only other activity producing this degree of effect was playing a musical instrument. In lockdown, I was recommended DUOLINGO. It's a free on-line language learning platform and offers around 20 languages, all the usual ones and some lesser known ones. It's very user-friendly, quite gimmicky but fun. You sign up to whatever time you want to give - I just commit to ten minutes a day, doing more when I feel like it. I've been going for 15 months.
I have just been made redundant and my immediate feeling was relief, I have been trying to keep up, and stay on top of things like the old me could, I was only diagnosed two years ago, but it seems MS has been around for me for at least 8years with many brain and spinal lesions. I am now in the situation of thinking what do I apply for? NHS jobs at my pay grade, or do I take a step down to lesser role that I might manage better, but will keep me active and ‘using it’…. I am fortunate to have protected my income with insurance prior to diagnosis, but I am 34 and not ready to ‘retire’ …. I think the cognitive element is really not addressed or spoke about enough. Thank you for your blog