Case study: managing active secondary progressive MS
A case of rapidly progressing secondary progressive MS despite treatment with rituximab. How to investigate and manage SPMS and at the same time managing expectations.
Case study
I am a 26-year old man who in Nov 2011 developed myelitis shortly after a vaccine. It started as a feeling of weakness and numbness in my left arm that then involved my left leg. I also had balance, bowel and bladder issues. With regular exercises, I gradually recovered to a point where I could run for 3 km at a stretch (85-90% recovery). However, minor bowel, bladder and balance issues persisted.

In March 2014 I noted some of my symptoms started getting worse. By March 2015 my balance, bowel and bladder issues worsened and I started experiencing spasms in my left leg and lower abdomen.
In September 2015 MRI of the brain and spine were done and I was diagnosed with RRMS. I was treated with methylprednisolone 1g intravenously for 5 days followed by treatment with dimethyl fumarate (Tecfidera). This was despite the feeling that I had already transitioned to the secondary progressive phase by the time I was diagnosed in 2015.
From September 2015 to October 2016 there was no radiological or clinical change.
From October 2016 to January 2018 my symptoms (mainly walking and bladder control) worsened.
The DMF was stopped in March 2018 due to falling WBC levels and a number of new lesions in the brain. At this stage, my diagnosis was changed to SPMS.
I decided to stop allopathic medicines as they seemed to be doing no good, except for the first year when I remained stable. However, following this brief period, I noticed gradual deterioration with my left leg becoming heavier and weaker with time.
From March 2018 to June 2018 I tried a host of alternative therapies, but nothing helped and walking in open areas without assistance became very difficult.
In June 2018 I was given another course of intravenous steroids followed by gradual tapering with oral prednisone for 21 days, which did not help much. The steroids seem to make my body stiffer and heavier.
My neurologists were planning to start natalizumab (Tysabri), but my JC virus test came back to be highly positive (JCV index = 3.84).
In July 2018 I saw a nutritionist who started low-dose naltrexone or LDN and I eliminated all grains, except rice, from my diet.
From July to October 2018, there was no worsening of symptoms, but a slight improvement in terms of energy levels and walking. Spasticity and heaviness in the left leg and lower back was difficult to cope with.
In November 2018 I again started deteriorating and started to use a walker.
In March 2019 I bought a laser therapy device and started using it.
From March 2019 to September 2019 my condition was more or less stable with no overt deterioration but also no improvement either.
In September 2019 I saw a neurologist who advised starting treatment with Rituximab, but since my WBC count was still very low due to the previous treatment with DMF I had to wait for 3 more months before starting rituximab in December 2019 and having a second dose in December 2020.
From December 2020 to now the stiffness in my lower back has gotten worse and my legs have become heavier. Standing has become much more difficult. At present, I can manage to walk only short distances using a walker when I'm feeling well. I have a feeling of heaviness and pain in my lower back, which increases exponentially after walking a few minutes. I have stiffness in both legs, which is significantly more on the left and I have bilateral foot drop. I also have difficulty keeping my torso straight and knees fully extended while standing. I have both poor bladder and bowel control. Fatigue is a big problem and I have body pain, spasms, restless legs and periodic leg movements while trying to fall asleep.
What are my treatment options?
Prof G’s Opinion
Firstly, your story is a familiar one, i.e. of a young man with an initial attack involving the spinal cord followed shortly by a relentlessly progressive deterioration in lower limb function with bladder and bowel function.
For the sake of the discussion I am going to assume you have MS and all MS mimics have been excluded. You are the kind of patient that needs an MS MOT*. The MOT will need to address all of your symptomatic problems as a result of the damage the MS has caused to your spinal cord. It seems as if you need the management of your bladder and bowels sorted out as well as your spasticity. You may find some of my previous MS-Selfie Newsletters, which deal with your symptomatic problems of help. I will do be doing Newsletters in the future on walking, spasticity, limb jerks and restless legs.
Help, I am peeing myself at night
It is clear that you need to see a physiotherapist. I suspect you need foot splints or possibly functional electric stimulators for your foot drop. This is not just to improve your walking, but to try and prevent falls and fractures.
Based on your email what you really want from me is to explain why you are getting worse and for me to stop your progression and reverse your disability. I would urge you to read the Newsletter ‘Getting worse’, which explains what is happening to your spinal cord.
What I would need to do is to see if your MS is active. This would involve me ordering an MRI of the brain and spinal cord with gadolinium-enhancement and comparing it with your earlier scans. If you had any enhancing or new lesions you would be eligible in my NHS practice of siponimod. If there is no evidence of MRI activity I would offer you a lumbar puncture to measure your spinal fluid neurofilament levels. If the neurofilament levels were raised I would offer you off-label subcutaneous cladribine as part of our compassionate use programme or recruitment into a clinical trial. As your current EDSS is 6.5, i.e. you need a walker (bilateral support) to walk 10m, you would be eligible for our CHARIOT-MS or SIZOMUS trials.
It is important for you to realise that you still have a lot of neurological functions to protect, in particular your arm and hand function, bulbar function (speech and swallowing) and your cognition. Our CHARIOT-MS is testing oral cladribine in more advanced disease (EDSS 6.5-8.5) with the primary outcome being upper limb function as assessed by the 9-hole peg test. The SIZOMUS trial is a safety study of Ixazomib, a CNS penetrant proteosome inhibitor, to try and scrub the brain clean of B-cells and plasma cells.
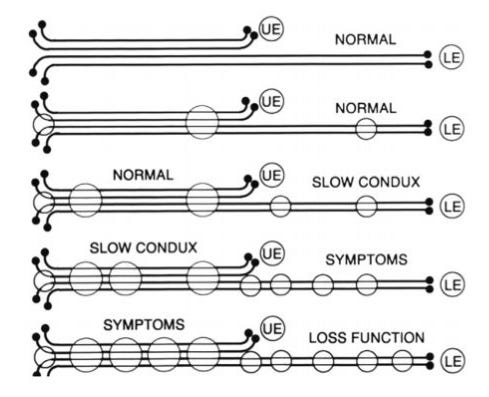
What many people in the MS community think is that once you have lost your lower limb function that your MS is beyond treatment and non-modifiable. We have challenged this dogma with our so-called length-dependent axonopathy hypothesis (Giovannoni, MSARDs 2017 Feb;12:70-78), i.e. the longest nerve fibres to the legs are hit most and degenerate first in MS. On the other hand, the shorter fibres to the upper limbs are less affected and hence more resilient to damage. These fibres still need protection with anti-inflammatory therapies.
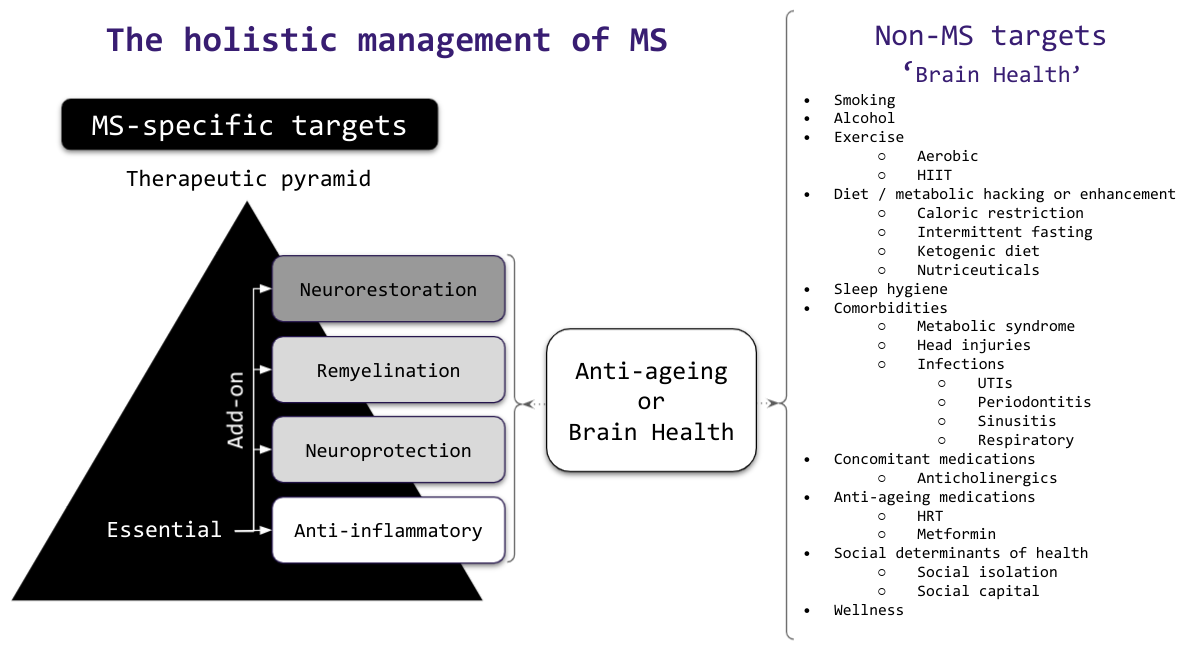
In the ‘Getting worse’ Newsletter I provide the rationale for testing add-on therapies, which include neuroprotectants, remyelination and neurorestorative therapies and treatments targeting putative mechanisms underlying smouldering MS. However, these strategies need to be tested in clinical trials and hence I am not in a position to recommend or offer them to you as part of routine clinical practice.
It is important to realise that there many other things that can potentially be done to slow down your MS progression and to improve your MS symptoms. I refer to this as the holistic management of MS.
I am just checking to make sure you are on vitamin D supplementation. Other issues that need checking are your mood, sleep, sexual function, cognition and dental and foot hygiene. Can I assume you don’t have pressure sores? What about your social health? Are you working, getting out and seeing family and friends? Social capital is critical to help pwMS adjust to their disability. What about exercise? I realise it is difficult but deconditioning contributes to fatigue and exercise may help improve many of your symptoms. Please don’t give up I have many patients who are very disabled who lead a very fulfilling life.
I want to thank you for your email and subscribing to MS-Selfie I hope some of the self-management tips are making a difference to you.
*An MOT is the Ministry of Transport’s requirement for every vehicle in the UK to have an annual service to make sure they are safe, roadworthy and to check their exhaust emissions are within national guidelines.
Subscriptions
Thank you all for subscribing to this Newsletter. The funds will be used to administer the Newsletter and MS-Selfie microsite. If you are reading this Newsletter and are not a paid-up subscriber, but you can afford to subscribe, I would urge you to do so. Subscriptions will help me and the MS community. I simply don’t have the time to do all the work myself. Please note If you can’t afford to subscribe and have MS, please drop me an email so that I can offer you a complimentary subscription.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.




https://www.healthline.com/health/secondary-progressive-ms/new-treatments ?!
I agree, I am glad you reviewed this case. I am profoundly humbled in reading this man’s experience. We each have personal struggles as patients but his course seems excessively harsh.
I too hope he has social and family support as engagement offers so many positive benefits- fun experiences, assistance with daily tasks, a focus outside-of-self, ideas and collaboration. Of all these I believe Fun - and maybe alongside this - Hope cannot be underestimated.
If he does not feel he has sufficient social support I encourage him to look online. He may find people who ‘get it’ in a way pw/oMS cannot understand. I used to use Shift.MS but I am unsure of how much it has changed with time.
Information is also SO important- so this MS Selfie and the regular Blog are key reads. MultipleSclerosisNewsToday.com has some good articles- especially on coping. They now also have a podcast but I cannot personally recommend (have not tuned in).
This Blog post from last year really helps express how life has changed:
https://multiple-sclerosis-research.org/2020/07/the-kingdom-of-the-sick/
I leave with my prayers for this man in finding the answers he seeks and a life in balance with his ever changing reality.