Atara Bio's EMBOLD study is negative
What does this mean for the EBV hypothesis of MS?
Some of you would have heard by now that Atara Bio’s phase 2 EMBOLD trial of ATA188 in non-active progressive multiple sclerosis was negative.
“The study did not meet the primary endpoint of confirmed disability improvement (CDI) by expanded disability status scale (EDSS) at 12 months compared to placebo. In addition, fluid and imaging biomarkers did not provide further supportive evidence. Atara said they were surprised and deeply disappointed with the results of EMBOLD, particularly for the MS patient community, which is in urgent need of new treatment options. Preliminary safety data showed no new safety signals in the EMBOLD study, reinforcing the favourable safety profile observed with ATA188.
Atara is reviewing the data, including a 6% disability improvement in the treatment arm compared to the 33% disability improvement observed in the Phase 1 study, in addition to identifying the factors related to a substantially greater than expected placebo rate of 16% for CDI at 12 months compared with an expected rate of 4-6% in non-active PMS patients.”
In summary, more study subjects in the placebo group (16%) improved compared to the treatment arm (6%).
You can read the full press release on Atara’s website.
The questions I have are: did this trial fail because (1) it was testing a wrong hypothesis, (2) it was poor science, (3) poor trial design, and (4) what do these results mean for the EBV hypothesis of MS?
The wrong hypothesis
The epidemiology supporting EBV as the cause of MS is very compelling. The data is so overwhelming that I have already accepted that EBV is the cause of MS, which is why we are pushing ahead with EBV vaccination as a way to prove that EBV is the cause of MS. However, the epidemiology tells us very little about how EBV causes MS. The critical question is whether EBV simply triggers MS (hit-and-run hypothesis) or does it drives the disease via latent-lytic cycling (driver hypothesis). The ATA188 Embold study tested the latter hypothesis, which may be incorrect. If this is the case, it means all of the preliminary work done by Michael Pender and the circumstantial evidence of increased latent-lytic cycling is wrong. I don’t buy this.
Poor science
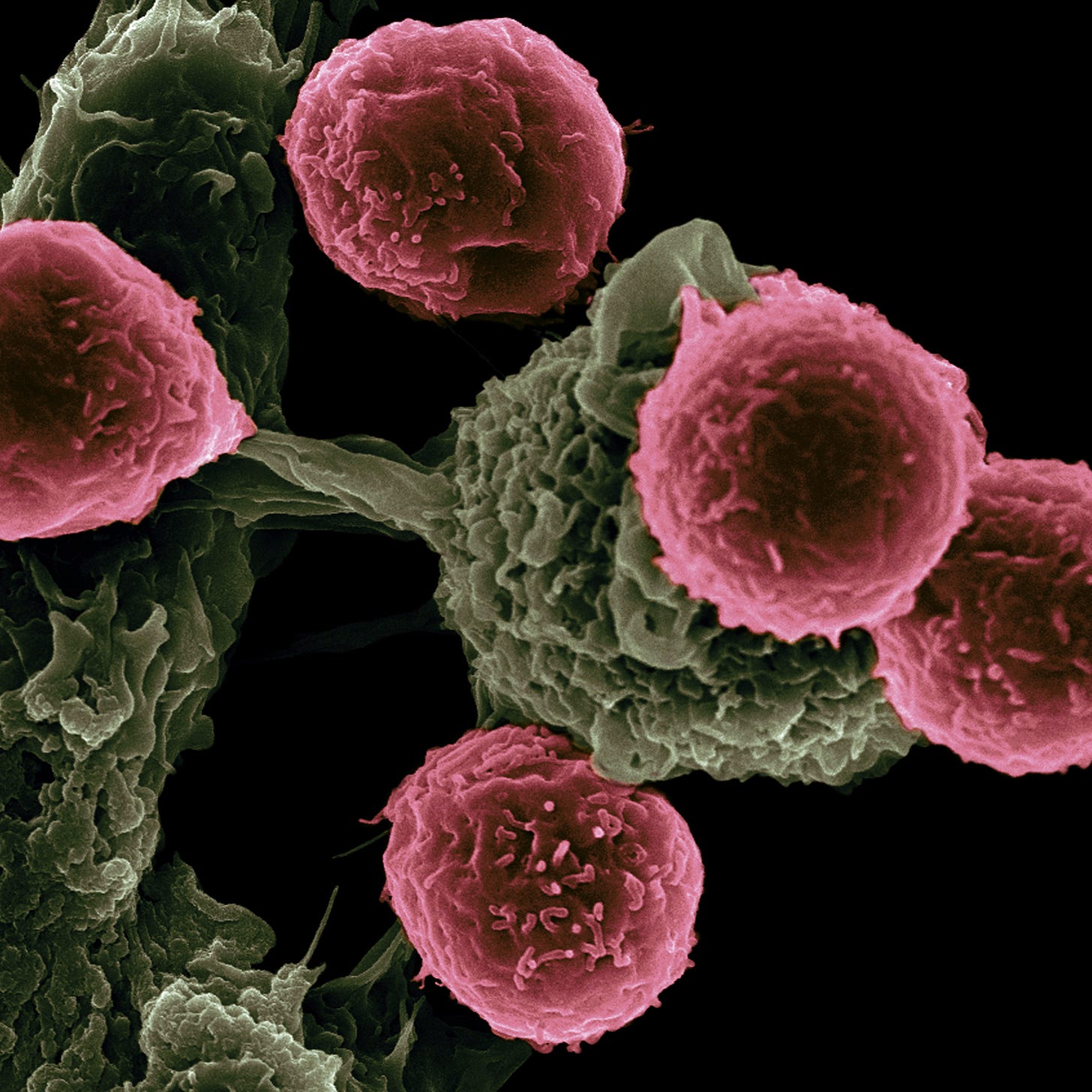
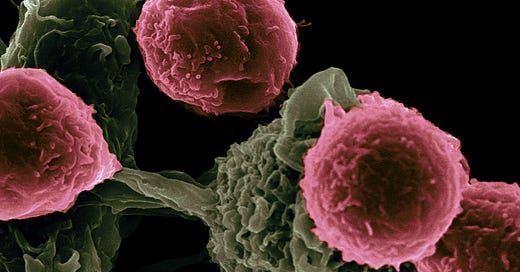
ATA188 are allogeneic (donor lymphocytes) that target EBV proteins. These cells express different HLA (human leukocyte antigens) and are selected based on HLA-types to prevent the recipient (trial subjects) from rejecting them. However, as the HLA matches were imperfect, we have yet to learn how well these cells survived in individual subjects.
The ATA188 development programme was based on work by Michael Pender’s group using autologous EBV-targeted CTLs (cytotoxic T-lymphocytes). Autologous cells are harvested from patients, and then EBV-specific cells are expanded and stimulated in the laboratory before being infused into the patient. As the HLA matching is not an issue, the expanded cells will likely survive better because they are autologous.
Atara has recently presented data showing that these cells survive after being infused, but whether they are activated and effective against EBV is unknown. EBV and other herpes viruses have developed elaborate molecular techniques for switching off T-cells targeting the cells they infect. This is how herpes viruses persist. It is critical to know if the ATA188 CTLs maintain an activated killing phenotype or whether or not they become senescent or non-reactive when transferred back into patients. This point is critical. The most significant recent cancer advancement has been immunotherapy with the so-called checkpoint inhibitors. The checkpoint inhibitors remove the molecular breaks on senescent T-cells, allowing them to identify and kill cancer cells. Is it possible that the ATA188 cells need the help of a checkpoint inhibitor or another stimulant once they are inside the body of someone with MS.? I sincerely hope Atara Bio allocates resources to look at this more thoroughly.
Do ATA188 cells control EBV in pwMS? To my knowledge, no work has been done in MS patients on whether ATA188 stops latent-lytic cycling of EBV and whether or not it reduces EBV viral loads. A simple experiment that could have been done before starting the phase 2 trial would have been to look at whether or not ATA188 stops EBV shedding in the saliva and reduces EBV viral loads in the peripheral blood B-cell compartment using new ultrasensitive PCR techniques. I can’t understand why this was not part of the ATA188 phase 1 programme. If ATA188 does not control latent-lytic cycling of EBV, why would one test it in MS?
Another issue is space for the cells to migrate into and survive. The immune compartment is a physical compartment with a finite amount of space. With some cell therapies, for example, CAR T-cells, you have to create space using a lymphodepletion cycle into which you transplant the cells. This lymphodepletion also acts as an immunosuppressive therapy, preventing the recipient from rejecting the engineered cells with a foreign receptor on their surface. I suspect a depletion cycle would help ATA188 cells survive, but we will never know, as Atara Bio is now unlikely to do this experiment.
Without answers to the above questions, we can’t say that ATA188 is an effective anti-EBV therapy in pwMS; therefore, we don’t know if ATA188 failed for this reason.
Atara Bio will counteract these criticisms by saying that this treatment strategy, i.e. allogeneic EBV-specific T-cells, works in patients with EBV-associated lymphomas; therefore, it should work against EBV in pwMS. However, the immune compartment and immunology of someone with a refractory B-cell lymphoma are likely to be very different from someone with MS. I am not convinced you can transfer what is seen in lymphoma patients to treating MS without some detailed immunological studies. Lymphoma patients typically have been immunosuppressed with chemotherapy and anti-CD20 therapies before receiving allogeneic EBV-targeted T-cells.
Poor trial design
Many in the field have criticised the Embold trial design because it was done in inactive progressive patients who were quite disabled and with little neurological reserve and capacity for recovery. This may be the case, but the Embold trial design was based on the progressive patients treated with autologous EBV-targeted CTLs by Michael Pender’s group. If Michael Pender’s results are anything to go by, the population of MS patients selected is irrelevant. On the other side is whether Michael Pender’s results are misleading.
The amazing placebo-response rate in the confirmed disability improvement of 16% in the Embold study tells you that despite having advanced MS, a large number of patients with progressive MS can recover function. Could the improvement in Michael Pender’s patients and the subjects in the ATA188 phase 1 trial be due to a placebo effect? These placebo results are yet another sobering example of how poor the EDSS is as an outcome in clinical trials. Based on these results, anyone targeting EBV with antivirals and/or immunotherapy would be advised to include patients in the earlier stage of the disease with less disability.
The debate about trial design and the patient population only becomes relevant if the underpinning science is good. As I explained above, the science underpinning this trial is not sound; therefore, the issue concerning trial design is a moot point.
What do these results mean for the EBV hypothesis of MS?
Hopefully, these results will have no impact on the EBV hypothesis. Without data on whether or not ATA188 impacts EBV biology in patients with MS, we can’t draw any conclusions from this negative study. If anything, the field should learn from this study and make sure that before we go ahead and look at any new anti-EBV antiviral or immunotherapy, we have some proof of biology to show that the treatment in question is impacting EBV in pwMS.
I am aware that these results will be very disappointing for the MS community, in particular for patients and researchers who are convinced EBV plays a role in the pathogenesis of MS. However, we must dissect the results of this trial and do a post-mortem of the immunology of ATA188 so we can learn lessons. I sincerely hope Atara Bio will allow this to happen and make available the biobank from the study for academics to explore some of the questions raised above.
Abstract
Introduction: In a Phase 1 open-label trial, treatment with ATA188, an off-the-shelf, allogeneic EBV-specific T-cell immunotherapy, was associated with confirmed disability improvement (CDI) in some patients with progressive MS, supported by less brain atrophy over time. Longitudinal monitoring of glial fibrillary acidic protein (GFAP), an emerging biomarker of progressing neurodegeneration expressed primarily in astrocytes, as well as ATA188-derived EBV-specific TCRβ-clonotypes may provide further mechanistic insights underlying ATA188-associated CDI.
Design/Methods: Plasma GFAP was measured longitudinally using SiMoA technology and then correlated with treatment time in subjects achieving CDI versus not; CDI versus stable versus confirmed disability progression (CDP). Deep sequencing of TCRβ-clonotypes was utilized as a tool to detect ATA188-derived EBV T cells following treatment.
Results: GFAP levels significantly increased during treatment in those not achieving CDI (n=17) but not the CDI group (n=7). Patients with CDP (n=4) showed significantly higher GFAP increases over time versus patients with CDI; there was no significant difference when comparing stable (n=13) versus CDI or stable versus CDP, although the latter showed a trend (Figure 1). Nineteen of 24 patients showed evidence of ATA188-derived EBV-specific TCRβ-clonotypes, with some exhibiting EBV-encoded LMP2A antigen (HLA A2-restricted, FLYALALLL)-specific reactivity. In some patients, ATA188-clonotypes were detected 2 months after receiving their final dose in year-1, which was the latest time point tested (Figure 2).
Conclusions: Data presented here show that CDI following ATA188 treatment appeared coincident with stabilization of GFAP, while patients with CDP showed significant increase in GFAP over time. Furthermore, ATA188-derived EBV-specific TCRβ-clonotypes were detected up to 2 months post-infusion.
Subscriptions and donations
MS-Selfie newsletters and access to the MS-Selfie microsite are free. In comparison, weekly off-topic Q&A sessions are restricted to paying subscribers. Subscriptions are being used to run and maintain the MS Selfie microsite, as I don’t have time to do it myself. You must be a paying subscriber if people want to ask questions unrelated to the Newsletters or Podcasts. If you can’t afford to become a paying subscriber, please email a request for a complimentary subscription (ms-selfie@giovannoni.net).
Important Links
X (Twitter) / LinkedIn / Medium
General Disclaimer
Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Queen Mary University of London or Barts Health NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.




Email:
For me its a combination of poor science, mode of action and trial design. In addition to what you propose EBV antibody titres should be checked (optimally serum and CSF), I hope we get to see that.
Oh wow, i can't believe it (!) :(
I guess curing ms just got postponed for another 50 years because no one will touch it now.