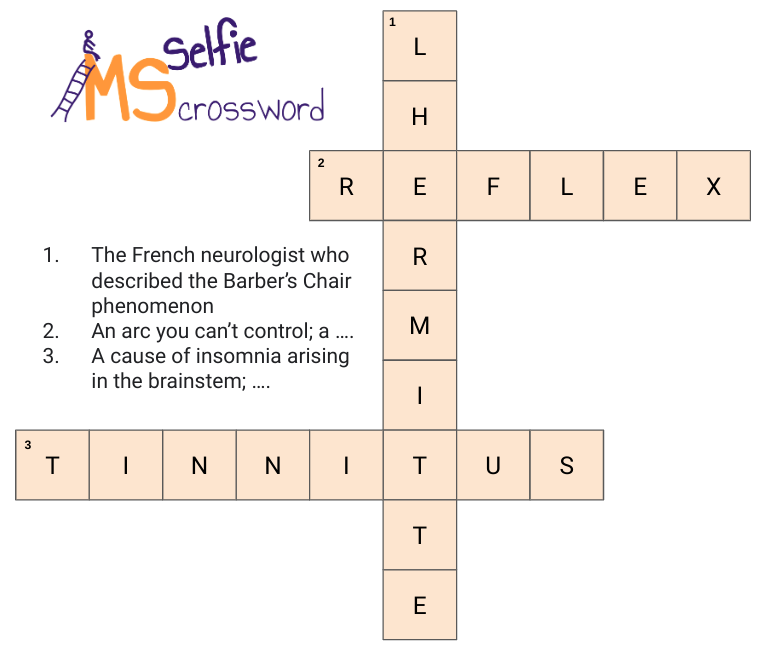
1. The French neurologist who described the Barber’s Chair phenomenon …
Lhermitte
Lhermitte's sign, which is also known as Lhermitte's phenomenon or barber chair phenomenon, describes an electric shock-like sensation that occurs on flexion (bending forward) of the neck. The shocklike sensation radiates down the spine and often into the legs, arms and occasionally around the body. Although Lhermitte described it in 1924 in a patient with MS it was actually first described by Marie and Chatelin in 1917 and in association with MS by Beriel and Devic in 1918.
Lhermitte's sign is actually a misnomer and should be called a symptom as it is a subjective experience and is not always associated with an abnormal clinical examination, i.e. objective findings, which is what is needed to define a sign.
Lhermitte's sign is due to a lesion in the so-called posterior sensory columns of the spinal cord. Although a demyelinating lesion is the commonest cause it can be caused by numerous other conditions. It is not an uncommon first manifestation of MS. Although it is an intermittent symptom that requires you to flex your neck to illicit it most neurologists would classify recent-onset Lhermitte's sign as a relapse despite it not fulfilling the strict definition of an MS relapse, i.e. ‘the appearance of new symptoms, or the return of old symptoms, for a period of 24 hours or more – in the absence of a change in core body temperature or infection’.
A lot of pwMS who have Lhermitte’s often flex their necks repeatedly to see if the symptom is still there. I suggest you don’t as this stretching is causing those demyelinated damaged nerve fibres to fire excessively that may cause them to degenerate faster. If you find Lhermitte's too uncomfortable or painful it can be treated with sodium channel blocking agents to reduce the firing of the damaged nerves. Sodium channel blockers include phenytoin, carbamazepine, oxcarbazepine and lamotrigine. Lhermitte’s phenomenon usually persists for about 4-6 weeks and gradually resolves like other relapses, but I have noted in several patients in whom it has persisted for months or even years.
2. An arc you can’t control; a ….
Reflex
The reflex arc is a special type of neural circuit that begins with a sensory neuron at a receptor, for example, a stretch receptor in a tendon) and results in an effect via a motor neuron, for example, contraction of a muscle. I assume you have all had your knee or ankle reflexes tested. If they are excessively brisk it is a sign of damage to the motor pathways. These tendon reflexes are very simple compared to more complex reflexes that control other neurological functions, for example, the pupil's response to light, eye movements, balance centres, coordination, etc. As a neurologist, I spend a lot of my time testing reflexes to see which part of the nervous system is damage or malfunctioning.
3. A cause of insomnia arising in the brainstem; ….
Tinnitus
Tinnitus is the name for hearing noises that are not caused by sounds coming from the outside world. Tinnitus is common in pwMS and is usually a sign of a lesion in the auditory pathways and may be associated with other brainstem symptoms and signs, for example, hearing loss, vertigo, unsteadiness of gait, sensory loss in the face, double vision, etc…
Acute onset tinnitus can occur as part of a relapse. MS-associated tinnitus may recover on its own when it is part of a relapse. Many pwMS complain that tinnitus is very uncomfortable and keeps them awake at night (insomnia). If the latter occurs using background white noise can help. White noise includes all frequencies audible to the human ear, i.e. between 20 and 20,000 hertz, played at an equal intensity or amplitude, to produce a "shh" sound similar to that of a humming air conditioner, a hair dryer, a whirring fan, TV static, or radio static.
It is important not to assume that isolated tinnitus in a patient with MS is due to MS disease activity. The patient needs to be examined and if necessary sent for audiology and ENT assessment to exclude other causes. I have several MS patients with comorbid Meniere’s disease and their tinnitus is not due to MS.
The prize winner
Sadly no reader managed to get tinnitus. So this week there is no prize winner.
Subscriptions and donations
Paid subscriptions to MS-Selfie are being used to administer the Newsletter and associated MS-Selfie microsite that is currently in development. At the request of several readers, I have now added the option of making a one-off donation. To keep this initiative open to all readers I would appreciate it if those who can afford a subscription to please subscribe. For active paying subscribers, thank you; your contribution is much appreciated.
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry or Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.





I cant believe i didn't see it cos i definitely hear it 😂😂😂 And omg did i rack my brains for no 3 😁
Funny I've never once thought of tinnitus as a cause of insomnia, but guess it must be. Thanks for putting us all out of crossword clue misery.