AHSCT vs. Alemtuzumab
The consequences of alemtuzumab being restricted as a treatment for active MS should not be underestimated.
When alemtuzumab was licensed by the FDA as a third-line disease-modifying therapy it ensured that problems would arise. People who get to alemtuzumab are very different to those starting it as a first-line therapy or early switch agent. Firstly, they had had MS longer, were older and had many more comorbidities. This meant they were much more likely to get adverse events. In summary, the FDA licensed alemtuzumab in a population that had really been studied in the pivotal trials. So nobody was surprised when a whole new set of serious adverse events emerged relating to the older, more disabled population. The main concerns were vascular complications such as myocardial infarction, stroke and intracerebral bleeding and a small number of cases with water on the lung due to a capillary leak syndrome or pneumonitis.

These new safety concerns caused the European Medicines Agency (EMA) to doubt its wisdom and run scared on alemtuzumab and let people with MS down. What the EMA forgot to take into account is how bad MS can be as a disease and that most of the early damage occurs occultly before people with the disease and their close ones realise the extent of the damage. What is lost in MS is lost forever. They also assumed that pwMS and the HCPs were not competent enough to assess risk; the EMA should be the final arbiter of risk. The latter is an interesting position because many pwMS who gave evidence to the EMA wanted alemtuzumab to keep its liberal label as a treatment for active MS. This is an example of authorities paying lip service to pwMS and ignoring their position.
Please be aware that we have no magic treatment that can repair the damage and turn back the clock, which is why the EMA’s Article 20 alemtuzumab review was so critical for the field. The regulator’s taking away the ability of pwMS to assess and weigh up their own risks and choose alemtuzumab first-line has turned back the clock. In the UK alemtuzumab can only be used as a first-line agent in patients with rapidly evolving severe (RES) MS (two disabling attacks in a 12 month period), which is now quite a small group of patients. I heard on Friday that maybe a handful of patients are now being treated with alemtuzumab in the UK annually. I personally think we may have thrown the baby out with the bathwater.
Early effective treatment in MS is about prevention; preventing the accrual of irreversible damage and giving pwMS the opportunity to age relatively normally. Now that alemtuzumab has become a 2nd- or 3rd-line option for pwMS many are seeking alternative treatment strategies and it has increased health tourism abroad for AHSCT. Is this what the EMA wanted or intended?
As AHSCT is a procedure and not a drug, it doesn’t require EMA or MHRA approval. Therefore, we should be actively pushing for AHSCT to become a 1st-line treatment option. If I had MS, why would I want to watch and wait whilst I failed one or two DMTs before getting to the very high efficacy IRTs (immune reconstitution therapies) that have the biggest impact on preventing end-organ damage, reversing disability, inducing long-term remission and possibly offering a cure? Interestingly, both alemtuzumab and HSCT are considered to be the most cost-effective DMTs available.
When asked which DMT would I choose if I had MS, I have started saying AHSCT. When I admitted this a few years ago, one of my patients, who I have been looking after for over a decade, sent me an email stating how upset she was that I had never offered her AHSCT. I clearly need to explain my position so as not to upset anyone else.
AHSCT is not on offer as a routine NHS therapy. At the moment AHSCT is only considered a 3rd-line treatment in the most active patients. Another problem is that it is not on offer across the country. There are only a handful of MS centres that are prepared to refer their patients for AHSCT. This means that access to AHSCT is not equitable and explains why an increasing number of patients travel abroad, at great personal cost, to receive this therapy.
The block in access to AHSCT seems to be at the level of the neurologist/MSologist. NHS England guidelines for bone marrow transplant (BMT) units allow their discretionary use of up to 15% of their AHSCT procedures to treat autoimmune conditions, which includes multiple sclerosis. As BMT units exist across the country access to these units would simply require a referral from a neurologist to the unit to request AHSCT as a treatment for MS. The latter, however, is unlikely to happen unless the local MSologist champions AHSCT as a procedure and get their local haematology unit on board. It always takes a local champion to make things happen.
Another factor that has changed in the last 10 years is the strength of the evidence demonstrating how effective AHSCT really is as a treatment for MS. The MIST trial, the first large randomised controlled trial, and several meta-analyses of AHSCT confirm that AHSCT is a very effective therapy. At the same time, the risks associated with AHSCT have improved and the mortality in most BMT units is now below 1% for MS. This has now tipped the scales in favour of AHSCT becoming a mainstream treatment for MS.
There is however resistance from the MS community about AHSCT being offered as first-line therapy. Why? I suspect because the risk: benefit profile of AHSCT has yet to be compared in a head-2-head study against our most effective licensed treatment, alemtuzumab. This is why we are starting a head-2-head study, the STAR-MS trial, of alemtuzumab or ocrelizumab vs. AHSCT in the hope of generating evidence. With the EMA making alemtuzumab 2nd/3rd-line this trial will almost certainly recruit too few patients on alemtuzumab for a direct comparison of alemtuzumab vs. AHSCT. I predict the majority of patients in the comparator arm will be on ocrelizumab. This would not be asking the same question as ocrelizumab is used as maintenance therapy and may in fact do very well against AHSCT; the trial is using clinical NEDA (no relapses or disease progression) as the primary clinical outcome. Ocrelizumab is pretty good in the short term at achieving clinical NEDA. For me, end-organ damage or brain volume loss in years 2 and 3, after rebaselining at 12 months, would be a much more informative outcome.
We know already that AHSCT will be more cost-effective than alemtuzumab and ocrelizumab, but will it be more effective and most importantly will it be safer? I suspect it may not be as safe in the short-term, but what about over a 10-20 year horizon? The one long-term AHSCT risk that worries everyone is the delayed secondary malignancy risk; cyclophosphamide that is used in both the stem cell mobilisation and ablation phases of AHSCT is a DNA alkylating agent and hence a mutagen. This is why long term follow-up data from the European Bone Marrow Transplant Registry will be so important to provide this information. The other downside of AHSCT is ovarian toxicity and infertility, which in my experience are the most common reasons for my patients saying no.
Please remember that most of the proponents of AHSCT as a treatment for MS recognise that the major benefits from treatment will only be derived if AHSCT is used early in the course of the disease. This explains why most BMT units don’t offer AHSCT to pwMS with more advanced, or progressive, MS. However, this has not stopped private, fee-for-service, units offering AHSCT to all-comers. If you have the money and are willing to travel abroad you will be able to find a BMT unit that will treat you. I think this is wrong and will not happen in the NHS if and when AHSCT becomes widely available. We have to be honest with our patients about the risks and the benefits of AHSCT and why we will limit AHSCT to those who will benefit the most. In fact, there is evidence that more advanced patients may actually be made worse by AHSCT; the chemotherapy used to ablate the immune system is neurotoxic and may speed up neuronal loss. In addition, serious life-threatening infections are more common when you have AHSCT, particularly in patients with more advanced MS, and infections are well known to worsen MS disability in more advanced MS.
Please be aware that AHSCT is not for the faint-hearted. It is a risky therapy with serious adverse events and quite a high mortality. Even an optimistic mortality rate of 0.3–0.5% is high when compared to licensed DMTs. Should this stop us from offering AHSCT first-line? I think not. If we have been prepared to offer alemtuzumab, with its risk profile as a first-line treatment, why not AHSCT? Most pwMS would agree that the decision regarding what is an acceptable risk to take should be taken by the patient and their families, and not the neurologist or other HCP. There is data showing that neurologists are much more risk-averse than pwMS. Neurologists need to acknowledge this bias, which is likely to be an unconscious bias, and let their patients make the decision.
What I am really trying to do by stating that if I had MS I would choose AHSCT as my treatment is to reframe the DMT debate, particularly in relation to access to highly effective DMTs. By focusing on AHSCT as a first-line treatment it should at least make you consider what your treatment objectives are in MS.
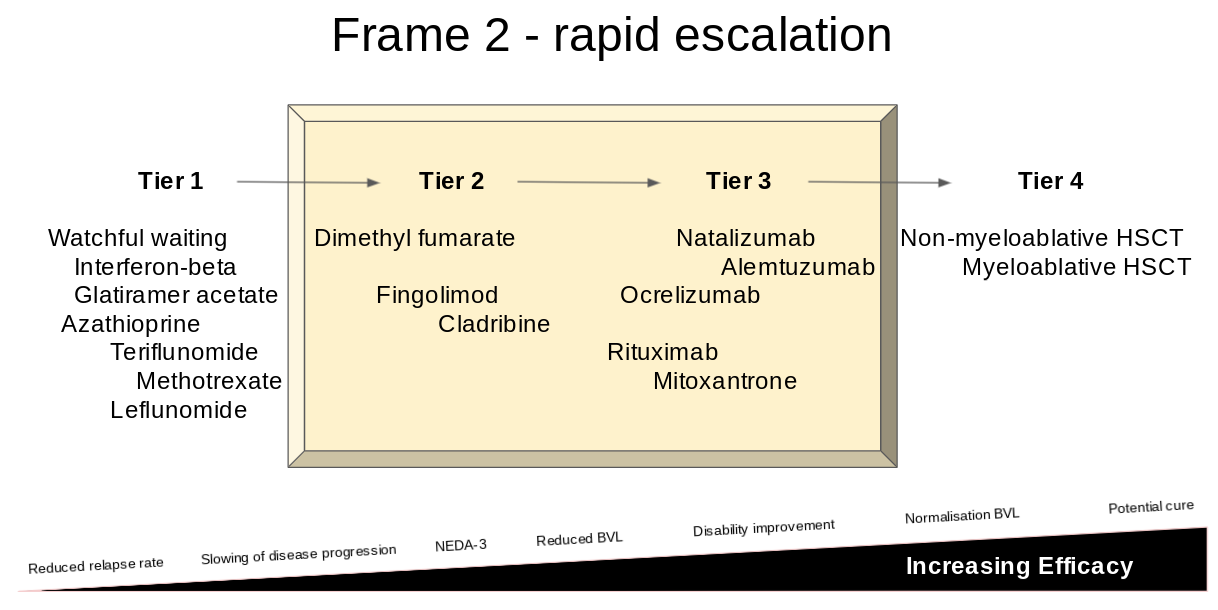
Framing is another cognitive bias that was identified by Daniel Kahneman, the Nobel laureate, and his partner Amos Tversky. By moving the frame upwards, or to the right, i.e to include AHSCT as a 1st-line therapy, it makes it more likely for pwMS and their neurologists to choose more effective, but arguably safer, treatments 1st-line.
We now know that people who start on a low to moderate efficacy DMT do worse on average than those who start on a high or very high efficacy therapy. Despite this, the majority of pwMS are not told this and are started on a low efficacy or platform DMTs without ever being given the option of a high efficacy DMT. Why? It is not due to lack of access to treatments as we now have several NICE and NHS England approved high efficacy DMTs available as first-line treatments.
So yes, if I had active MS I would want to have the full spectrum of high-efficacy DMTs available to choose from including AHSCT. I would like to know about their relative efficacy and what the aim of the treatments are. I would certainly want to have a discussion about the possibility of a potential cure.
By reframing the spectrum of efficacy by including AHSCT within the frame we may nudge pwMS and their neurologists to move up the treatment ladder and choose a high efficacy DMT sooner when they have more brain to protect.
Unfortunately, AHSCT as a first-line option is not going to happen any time soon, unless the MS community starts debating the issue in earnest. I am not alone, or out on a limb with my position; I have a short, but growing list, of MSologists who have told me that if they had MS they would want AHSCT first-line. If your MSologist would like his/her MS treated with AHSCT, why wouldn’t you?
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.






At last! As a person with MS (PPMS) and a long-term proponent of HSCT who has long been frustrated by the stand taken by many neurologists, I applaud your current reasoning.
My neurologist in Oxford told me seven years ago that I would be brought back in a box in I had HSCT. My haematologist in Oxford told me seven years ago that he couldn't understand why neurologists weren't referring their MS patients to him for HSCT. He supported my decision to have HSCT, especially as at that time there was no other treatment offered to me, and my condition was deteriorating. So I was the third British MS patient to travel to Russia for HSCT. Hundreds followed in my footsteps. I am currently seven years free from progression, and will be forever grateful that I was able to have HSCT, despite the cost.
I'm afraid that I must disagree that "all comers" are accepted for HSCT abroad because I can tell you that every single patient goes through extensive testing to ensure their fitness to undergo HSCT. Not everyone is accepted. I'm very happy that I was.
I can't thank you enough for the extraordinary work you conduct !!!
Having MS for 21 years and knowing lots of pwMS I can only agree with your perspective towards MS thérapies, we must go hard and as soon as possible to have an early stop in disease progression!
Even without access to AHSCT or HSCT if treatments like Alemtuzumab or Cladribine could be administered as 1st line therapy there would be two big advantages:
1st - stopping progression when there's very few irreversible lesions
2nd - pwMS receiving these IRTs at younger age would have more "strength" ( physically, psychologically, and others) to better mitigate possible side effects.