AHSCT or HSCT as a treatment for MS
What is AHSCT and what is involved when using it as a treatment for multiple sclerosis?
AHSCT = autologous hematopoietic stem cell transplant
HSCT = hematopoietic stem cell transplant
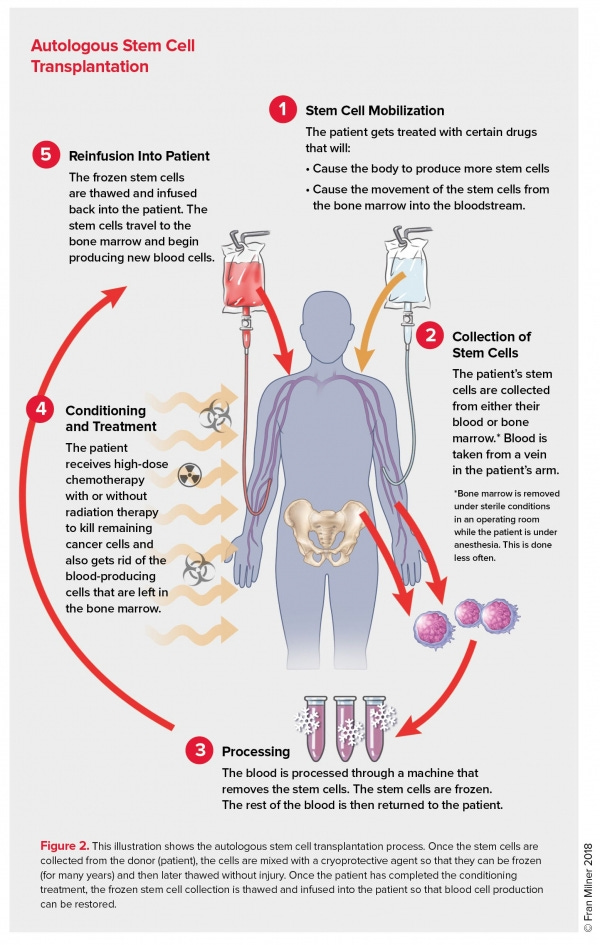
AHSCT is a rebranding of bone marrow transplantation or BMT. BMT was the term we used when the stem cells had to be harvested by doing bone marrow aspirates, i.e. a thick needle was inserted into the bone and the marrow sucked out under pressure. This procedure is painful and is done under sedation. I remember it very well when I was a houseman and junior medical registrar, or trainee, I worked on a haemoncology unit and had to do this procedure myself. Fortunately, haematologists have now developed an effective way of mobilising and harvesting stem cells from the blood without having to tap the bone marrow. This is done by giving a small dose of chemotherapy followed by growth factors so that the stem cells spill over from the bone marrow into the blood. These stem cells are harvested and frozen and can then be given after immunoablation therapy. Immunoablation therapy refers to chemotherapy to get rid of your immune cells.

Please note that all that these stem cells do is allow you to receive more potent chemotherapy and they work by allowing your bone marrow to recover more quickly. There is nothing magic about this; AHSCT in the treatment of MS is simply used to speed up bone marrow recovery, nothing more and nothing less. More rapid bone marrow recovery makes BMT safer. What causes patients to die from the procedure is usually so-called neutropaenic sepsis from not having enough white blood cells to fight infection.
To the best of our knowledge, these stem cells in AHSCT don’t go to the brain and spinal cord to repair the damage. This is a common misperception. People think the haemopoietic stem cells are being given to repair the damage that has accrued from having MS. This is why AHSCT, like other DMTs, is more effective when used early before MS causes too much damage.
There are different intensities of bone marrow ablation therapy. So-called myeloablative therapy is aimed at wiping out your immune system completely and replacing it with a new immune system. Non-myeloablative therapy is less intense in that it simply depletes your immune system partially and allows it to be rebooted (partially). The non-myeloablative therapy is clearly less risky than myeloablative therapy but less effective. In other words, more pwMS have a recurrence of their disease activity after non-myeloablative AHSCT, when compared to ablative-AHSCT. The chemotherapy that is used for non-myeloablative AHSCT is less toxic. Many in the field believe that if you are going to treat MS with AHSCT you need to go the more aggressive route and use the more toxic and risky ablative AHSCT. They argue that non-myeloablative AHSCT is not really better than the current high-efficacy drugs we are currently using to manage MS, i.e. alemtuzumab/cladribine and/or natalizumab and/or ocrelizumab/ofatumumab. This is why we are proposing to do a trial comparing alemtuzumab/ocrelizumab/cladribine with non-myeloablative AHSCT to see if non-myeloablative AHSCT is more efficacious and to see if the potential benefits of AHSCT warrant the risks. The study is called the STAR-MS study.
What are the risks of non-myeloablative AHSCT? The chances of dying from the non-myeloablative AHSCT is in the order of 0.3%-2%; i.e. 1-in-330 to a 1-in-50 chance of dying. Then there is the toxicity associated with the chemotherapy; nausea, vomiting, diarrhoea, hair loss, bleeding, infections, infertility and neurotoxicity to name a few. It seems that the more disabled you are, the worse the neurotoxicity. If you have lost a lot of nerve fibres already and have reduced brain reserve you handle chemotherapy poorly. The chemotherapy worsens neurological function. This is why a large number of BMT units stopped using this therapy in people with more advanced MS and is the reason why most units have an upper EDSS limit as part of their inclusion criteria.
Once your immune system recovers post-AHSCT does not mean it is necessarily back to normal. There is evidence that AHSCT may result in a rejuvenation of your immune system and changes the so-called repertoire of your B and T cells. At the moment we don’t know if this is a good or bad thing and what it means for MS. What we do know is that AHSCT destroys memory cells from your previous vaccinations. This is why you have to be revaccinated with all your childhood vaccines ~2 years after AHSCT to restore your immune responses to these common infections. Please note that not all BMT units demand revaccination; it depends on how ablative your HSCT is.
What about secondary autoimmunity? There is data in the literature that pwMS treated with AHSCT are at risk of developing secondary autoimmune diseases similar to that which occurs after alemtuzumab treatment, albeit at a slightly lower level. This is why it is hard to recommend non-myeloablative AHSCT, over alemtuzumab, outside of a controlled trial. It is easier to recommend AHSCT in a patient who has already failed alemtuzumab.
What about ablative AHSCT? This now is a different beast compared to non-myeloablative AHSCT in that the short-term risks associated with the intense chemotherapy needed to ablate the immune system are so much worse. Everything is worse; the diarrhoea tends to be bloody and protracted, mucositis is the norm (the lining of your mouth, throat and intestine slough), infections are more severe, and are potentially life-threatening, there is solid organ toxicity (liver, lungs, kidneys and heart), your bone marrow takes longer to recover and a result you are more likely to need platelet and blood transfusions. ablative AHSCT is not for the faint-hearted. A large number of AHSCT enthusiasts in the autoimmune field are of the opinion ablative AHSCT is the way to go; the failure rate from non-myeloablative AHSCT is too high. They argue that if you are going to take the risk, you might as well go for maximum efficacy.
The seemingly miraculous treatment effects with AHSCT, for example of people in wheelchairs getting up and walking, is not unique to AHSCT. We see these ‘Lazarus effects’ with other highly effective DMTs. Provided you have sufficient reserve capacity in the brain and spinal cord you will see spontaneous recovery from relapse-related disability once inflammation is switched off and recovery mechanisms are allowed to proceed. Tragically these Lazarus-like examples create unrealistic expectations for pwMS with more advanced MS. Once you have fixed or progressive disability it is likely that you have lost your neurological reserve and hence even if you switch off inflammation with AHSCT, or any other anti-inflammatory DMT for that matter, it is unlikely that there will be a significant recovery of function. This is one reason why so many progressive MS trials have failed in the past. Therefore the benefit-risk ratio changes with more advanced disease and it's the reason why most BMT units have age and disability cut-offs for pwMS.
Would I refer to pwMS for AHSCT? Yes, I do. The situation where AHSCT is indicated as part of routine clinical care is in the occasional patient with more malignant disease, who have failed licensed high-efficacy treatment options. In these patients, the benefits of AHSCT potentially outway the risks of the disease.
In practice, I find the main reason why pwMS say no to AHSCT is the infertility risk. The risk of premature ovarian failure, or early menopause, is over 40% and a lot of women when they hear this figure they tend to say no. Similarly, for males, the cyclophosphamide is toxic to the testes so if you want to start, or extend, your family you need to bank sperm.
Please remember the human brain is hard-wired to be optimistic. I like to use the gambler’s dilemma as an analogy. No gambler places a bet, or goes into a casino, to lose money; they always believe they are going to be the one that wins the jackpot. No person will sign-up to AHSCT believing that they are going to die or develop complications. However, there will always be the unlucky ones who have serious complications and occasionally die from the procedure, or develop serious delayed adverse complications. If you decide to have AHSCT as part of a trial, or as part of routine care, you need to ask yourself the question what if I am the unlucky one? Am I ready to leave my family and loved ones prematurely? If you answer yes, and yes, then you are ready to take the risks. In the same way, I always tell my patients who sign-up for alemtuzumab treatment that they should expect to develop a secondary autoimmune complication; if they don’t they should count themselves lucky. If they are not prepared to develop a second autoimmune disease then they shouldn't be treated with alemtuzumab.
Please note that AHSCT is NICE approved for the treatment of MS in the NHS. To access AHSCT your treatment decision needs to be approved via an MDT (multidisciplinary team) meeting and you then need to be referred to the BMT unit that is treating patients with MS and other autoimmune diseases. Despite NICE approval for BMT units to treat MS, access to AHSCT is very patchy in the UK.
Please note that I do think the data supports AHSCT as being the most effective treatment we have for MS. However, this is not really the question. The main question the MS community needs to answer is whether or not the risks are justified and who should be taking the risks?
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust. The advice is intended as general advice and should not be interpreted as being personal clinical advice. If you have problems please tell your own healthcare professional who will be able to help you.




Hello,
I know a few patients who have shown further progression (without MRI activity) after having aHSCT therapy. Is this a case of "smouldering MS" and would further treatment would you consider?
What are your thoughts on Mesenchymal stem cell therapy to treat MS? Is the research ongoing or going nowhere?